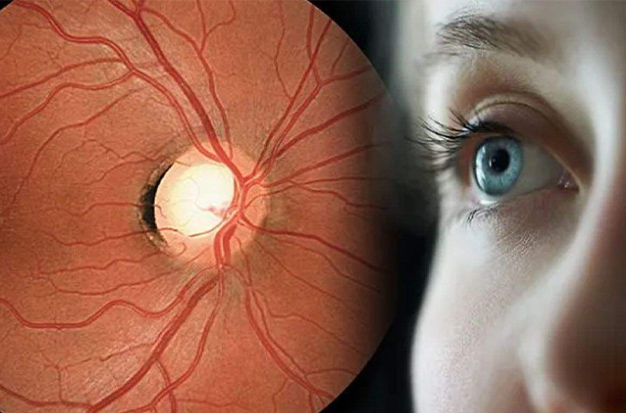
Affecting almost 3 million people in the United States., glaucoma is one of the most serious eye diseases and is a leading cause of blindness. Glaucoma doesn’t cause pain when it has its first signs, so many people don’t find out they have it until it’s advanced. Many glaucoma sufferers wonder if their condition can be reversed because it is brought on by increased pressure inside the eye, which harms the optic nerve. Yes and no are frequently both acceptable answers.
Is Glaucoma Reversible?
The answer to this query is no. The damage already done in terms of vision loss cannot be undone once glaucoma has been diagnosed in a patient because there is currently no treatment that can reverse the condition. But that does not imply that a patient should give up.
Treatment Of Glaucoma
Glaucoma harm cannot be undone. However, if you catch the disease in its earliest stages, treatment and routine checkups can help slow or prevent vision loss.
Your eye pressure (intraocular pressure) is reduced in order to treat glaucoma. Prescription eyedrops, oral medications, laser surgery, or a combination of any of these may be your options, depending on your circumstances.
Eyedrops
Eyedrops on prescription are frequently used to begin glaucoma treatment. These can aid in lowering eye pressure by enhancing fluid drainage from the eye or by reducing the amount of fluid your eye produces. You might need more than one of the eyedrops listed below, depending on how low your eye pressure needs to be.
The following are some examples of prescription eyedrops:
- Prostaglandins. These increase aqueous humor (the fluid in your eyes) outflow, which lowers eye pressure. Latanoprost (Xalatan), travoprost (Travatan Z), tafluprost (Zioptan), bimatoprost (Lumigan), and latanoprostene bunod (Vyzulta) are medications in this category. Mild eye reddening and stinging, iris darkening, eyelash or eyelid skin pigment darkening, and blurred vision are all potential side effects. One dose per day is recommended for this group of medications.
- Beta blockers. These lessen the flow of fluid into your eyes, which lowers intraocular pressure. Timolol and betaxolol, for instance, are examples (Betimol, Istalol, Timoptic). Breathing issues, a slowed heartbeat, low blood pressure, impotence, and fatigue are all potential side effects. Depending on your condition, this class of medication may be prescribed for once or twice daily use.
- Alpha-adrenergic agonists These cause your eye’s fluid to come out more quickly and produce less aqueous humor. Apraclonidine (Iopidine) and brimonidine (Alphagan P, Qoliana) are two examples. An irregular heartbeat, high blood pressure, fatigue, red, itchy, or swollen eyes, and dry mouth are examples of potential side effects. This class of medication is typically prescribed for twice-daily use, but it may also be prescribed for three times per day.
- Blockers of carbonic anhydrase. These drugs lessen the flow of fluid into your eyes. Brinzolamide (Azopt) and dorzolamide (Trusopt) are two examples. Frequent urination, a metallic taste, and tingling in the fingers and toes are a few potential side effects. This class of medication is typically prescribed for twice-daily use, but it may also be prescribed for three times per day.
- Rho kinase inhibitor. By inhibiting the rho kinase enzymes that cause fluid accumulation, this medication lowers eye pressure. It is prescribed for use once daily and is sold under the brand name netarsudil (Rhopressa). Eye redness, discomfort, and deposits forming on the cornea are examples of potential side effects.
- agents that are cholinergic or miotic. These increase the amount of fluid that drains from your eye. Isopto Carpine’s pilocarpine is one illustration. Headache, eye pain, smaller pupils, potential blurred or dim vision, and nearsightedness are some of the side effects. Up to four doses of this class of medication are typically recommended each day. These medications are no longer prescribed very frequently due to the possibility of side effects and the requirement for frequent daily use.
You might experience some side effects unrelated to your eyes because some of the eyedrop medication is absorbed into your bloodstream. For one to two minutes after applying the drops, keep your eyes closed to reduce this absorption. To stop the tear duct from opening for a minute or two, you can also lightly press on the corner of your eyes close to your nose. Clear your eyelid of any drops that aren’t being used.
If you must use artificial tears or have received more than one prescription for eyedrops, space them out so that there is a minimum of five minutes between each type of drop.
Oral Medications
Your doctor might also suggest an oral medication, typically a carbonic anhydrase inhibitor, if eyedrops by themselves are unable to lower your eye pressure to the desired level. Numerous side effects, such as frequent urination, tingling in the fingers and toes, depression, stomach upset, and kidney stones, are possible.
Surgery And Other Therapies
Additionally, there are surgical techniques and laser therapy. The following methods aim to enhance fluid drainage from the eye, thereby reducing pressure:
- Laser therapy. If you have open-angle glaucoma, one treatment option is laser trabeculoplasty (truh-BEK-u-low-plas-tee). It takes place in the doctor’s office. The trabecular meshwork’s blocked channels are opened by your doctor using a tiny laser beam. Before this procedure’s full impact is felt, it might take a few weeks.
- Filtering surgery. Your surgeon makes an incision in the sclera, the white of the eye, and removes a portion of the trabecular meshwork during a procedure known as a trabeculectomy (truh-bek-u-LEK-tuh-me).
- Drainage tubes. To lower your eye pressure, your eye surgeon will perform a procedure in which a tiny tube shunt is inserted into your eye.
- glaucoma surgery that is only minimally invasive. Your doctor may suggest a MIGS procedure to lower your eye pressure. Compared to trabeculectomy or placing a drainage device, these procedures typically require less immediate postoperative care and carry fewer risks. With cataract surgery, they are frequently combined. There are a number of MIGS techniques available, and your doctor will discuss which procedure may be right for you.
You must visit your physician for follow-up exams after your procedure. Additionally, you might eventually require additional procedures if your eye pressure starts to increase or if other changes take place in your eye.
Treating Acute Angle-closure Glaucoma
An emergency situation exists with acute angle-closure glaucoma. The pressure in your eye must be reduced immediately if you are diagnosed with this condition. Typically, this will necessitate both medication and laser surgery or other types of surgery.
You might undergo a procedure called a laser peripheral iridotomy in which the doctor uses a laser to make a tiny hole in your iris. Pressure on the eyes is reduced as a result of the fluid (aqueous humor) flowing through it.

Several Potential Avenues
Optic Nerve Cell Regeneration
The hope is that one day we will be able to restore vision that has been lost because of the death of retinal ganglion cells in those who have experienced very significant vision loss from glaucoma. Since these nerve cells do not typically regenerate, we must insert new nerve cells where the old ones were, connect them to the other retinal nerve cells from which they typically receive information, and develop a fiber up to the brain’s subsequent vision relay station. Making connections that result in useful vision while avoiding disrupting already-existing connections is necessary for the vision that hasn’t already been lost.
Innovative Drug Delivery And Neuroprotection
Patients would no longer require daily eye drops if glaucoma medication could only be administered once or twice a year. In order to slow the progression of glaucoma damage, a variety of agents could be injected into or applied to the eye, such as long-lasting medications that lower eye pressure or modified virus particles that insert new genes into the eye cells.
In-lab tests of glaucoma gene therapy have already been completed successfully. Neuroprotection, a term used to describe a number of strategies, includes gene therapy. There are a number of potential neuroprotective medications, but no conclusive benefit has yet been demonstrated in human trials.
Initial Steps
25 years ago, scientists thought it would be impossible ever to restore vision in glaucoma. Since then, some initial research steps have been completed. From a patient’s own eye, we can harvest new nerve cells. We can safely remove some of these progenitor cells and then use those to grow thousands of additional ones (Figure 1). Since they are the patient’s own cells, there won’t be any rejection issues.
Figure 1: Growing in a culture dish are new progenitor cells derived from eye cells already present. These could one day be the replacement cells required to restore vision lost to glaucoma.
Both eye and bone marrow progenitor cells have been tested as replacements in the eye and have briefly resided there.
The next step is to attach them to the retina’s already-existing cells and develop a fiber that ascends to the brain. In order to connect the eye and brain, we think that a piece of a nerve will be used to provide a pathway for the new fibers.
Lifestyle And Home Remedies
These recommendations could aid in lowering high eye pressure or enhancing eye health.
- Eat a healthy diet. While maintaining a healthy diet can help, it won’t stop glaucoma from getting worse. Zinc, copper, selenium, antioxidant vitamins C, E, and A, as well as other vitamins and nutrients, are crucial for maintaining eye health.
- Exercise safely. Open-angle glaucoma eye pressure may be lowered with regular exercise. Discuss a suitable exercise regimen with your doctor.
- Limit your caffeine. Caffeine-rich beverages may make your eyes more sensitive to pressure.
- Drink water frequently. Throughout the course of the day, only ingest small amounts of fluids at a time. Any liquid consumed in excess of a quart in a short period of time may temporarily raise eye pressure.
- Elevate your head while you sleep. It has been demonstrated that using a wedge-shaped pillow while you sleep lowers intraocular pressure by keeping your head raised by about 20 degrees.
- the use of prescribed medication. You can get the best outcome from your treatment by using your eyedrops and other medications as directed. Utilize the drops exactly as directed. If not, the damage to your optic nerve might get worse.



